How to Become an Animal Osteopath: Complete Career Guide
The path to becoming an animal osteopath combines professional expertise in animal health with specialized training in classical structural osteopathy—creating rewarding careers that bridge manual therapy and veterinary collaboration. For healthcare professionals, veterinarians, and animal therapy practitioners exploring how to become an animal osteopath, understanding animal osteopathy requirements, certification pathways, and career prospects provides the foundation for informed decisions about this expanding field.
This comprehensive guide examines the complete journey to animal osteopathy certification, explores animal osteopath salary expectations and career opportunities, reviews animal osteopathy schools and program options, and addresses practical considerations for professionals transitioning into this specialized discipline.
Understanding Animal Osteopathy as a Professional Field
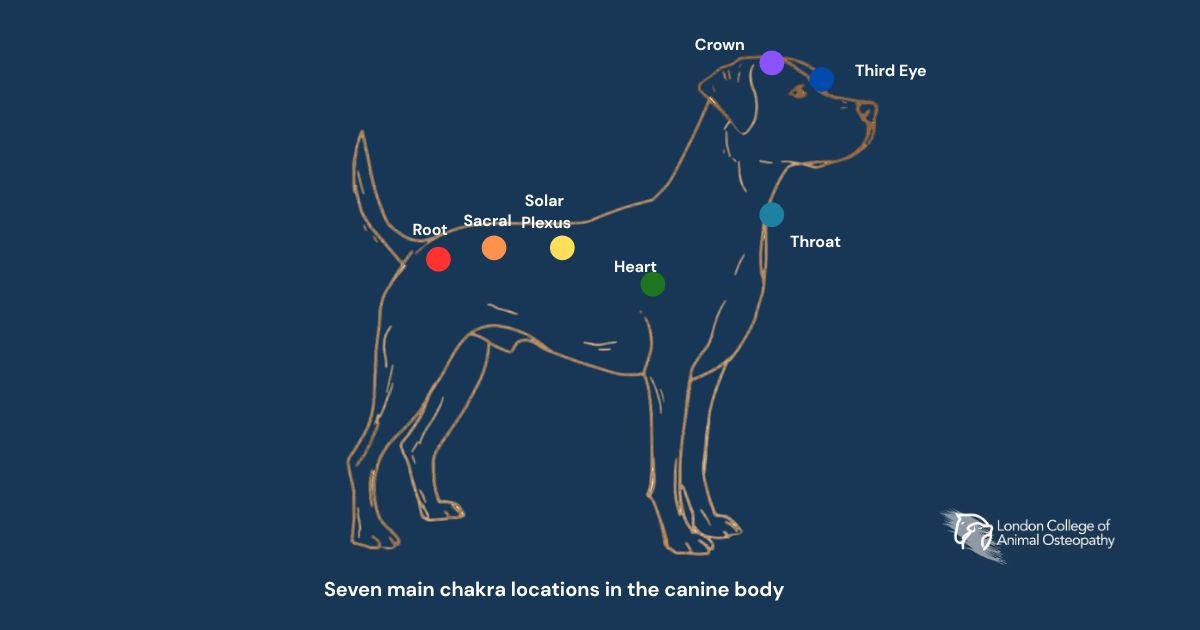
Animal osteopathy applies classical structural osteopathic principles—originally developed for human healthcare—to diagnose and treat musculoskeletal dysfunction in animals. Practitioners use precise manual techniques assessing tissue texture, symmetry, range of motion, and tenderness to identify restrictions, then apply specific interventions restoring optimal biomechanical function.
Scope of Practice and Clinical Applications
Animal osteopaths address diverse conditions affecting equine and canine patients, as detailed in resources about what animal osteopathy encompasses:
Performance Enhancement: Working with athletic horses and competitive dogs to optimize biomechanical efficiency, prevent injury, and support peak performance capabilities
Pain Management: Addressing chronic musculoskeletal discomfort from conditions like hip dysplasia in dogs or back pain in horses through manual techniques, reducing tissue restriction and inflammation
Injury Rehabilitation: Supporting recovery from orthopedic injuries, soft tissue trauma, or post-surgical healing by maintaining mobility and preventing compensatory patterns
Preventive Care: Regular osteopathic assessment and treatment prevent minor restrictions from progressing to performance-limiting or painful conditions
Geriatric Support: Enhancing quality of life for senior dogs through gentle techniques, maintaining mobility and comfort as degenerative changes develop
Behavioral Applications: Addressing pain-related behavioral issues by resolving underlying musculoskeletal dysfunction, creating discomfort
Professional Positioning and Veterinary Collaboration
Animal osteopaths function as complementary healthcare providers working alongside veterinarians rather than replacing conventional veterinary care. Successful practitioners develop collaborative relationships with veterinary professionals, receiving referrals for cases benefiting from manual therapy intervention while referring cases requiring veterinary diagnosis, pharmaceutical management, or surgical intervention.
This collaborative model distinguishes animal osteopathy from veterinary medicine itself—osteopaths address biomechanical function through manual techniques while veterinarians diagnose disease, prescribe medications, perform surgery, and provide comprehensive medical care.
 Manual osteopathic treatment is being applied to a dog, demonstrating hands-on assessment of musculoskeletal function
Manual osteopathic treatment is being applied to a dog, demonstrating hands-on assessment of musculoskeletal function
Animal Osteopathy Requirements: Professional Prerequisites and Eligibility
Unlike entry-level healthcare programs accepting students with minimal background, animal osteopathy schools require applicants to demonstrate established expertise in animal sciences, healthcare, or manual therapy. This prerequisite structure reflects the field’s positioning as advanced professional development rather than foundational training.
Eligible Professional Backgrounds
Veterinary Professionals:
- Veterinarians (DVM/VMD) seeking to expand treatment modalities beyond conventional approaches
- Veterinary technicians and nurses with clinical experience
- Veterinary rehabilitation specialists are adding manual therapy skills
Animal osteopathy certification enables veterinary professionals to offer integrated care combining their diagnostic expertise with manual therapy techniques, creating comprehensive treatment protocols as discussed in resources on enhancing veterinary care with osteopathy.
Manual Therapy Practitioners:
- Osteopaths (DO) or osteopathic manual therapists (OMT) transitioning from human to animal practice
- Physiotherapists with musculoskeletal specialization
- Chiropractors seeking to expand into animal healthcare
- Massage therapists with advanced training and animal experience
These professionals bring existing manual therapy expertise, requiring adaptation to quadruped anatomy and biomechanics rather than learning manual skills from scratch.
Animal Healthcare Specialists:
- Equine or canine massage therapists with established practices
- Certified rehabilitation practitioners (CCRP, CERP)
- Animal physical therapy providers
- Bodywork specialists (Masterson Method, Bowen Technique, myofascial release)
Experienced Animal Professionals:
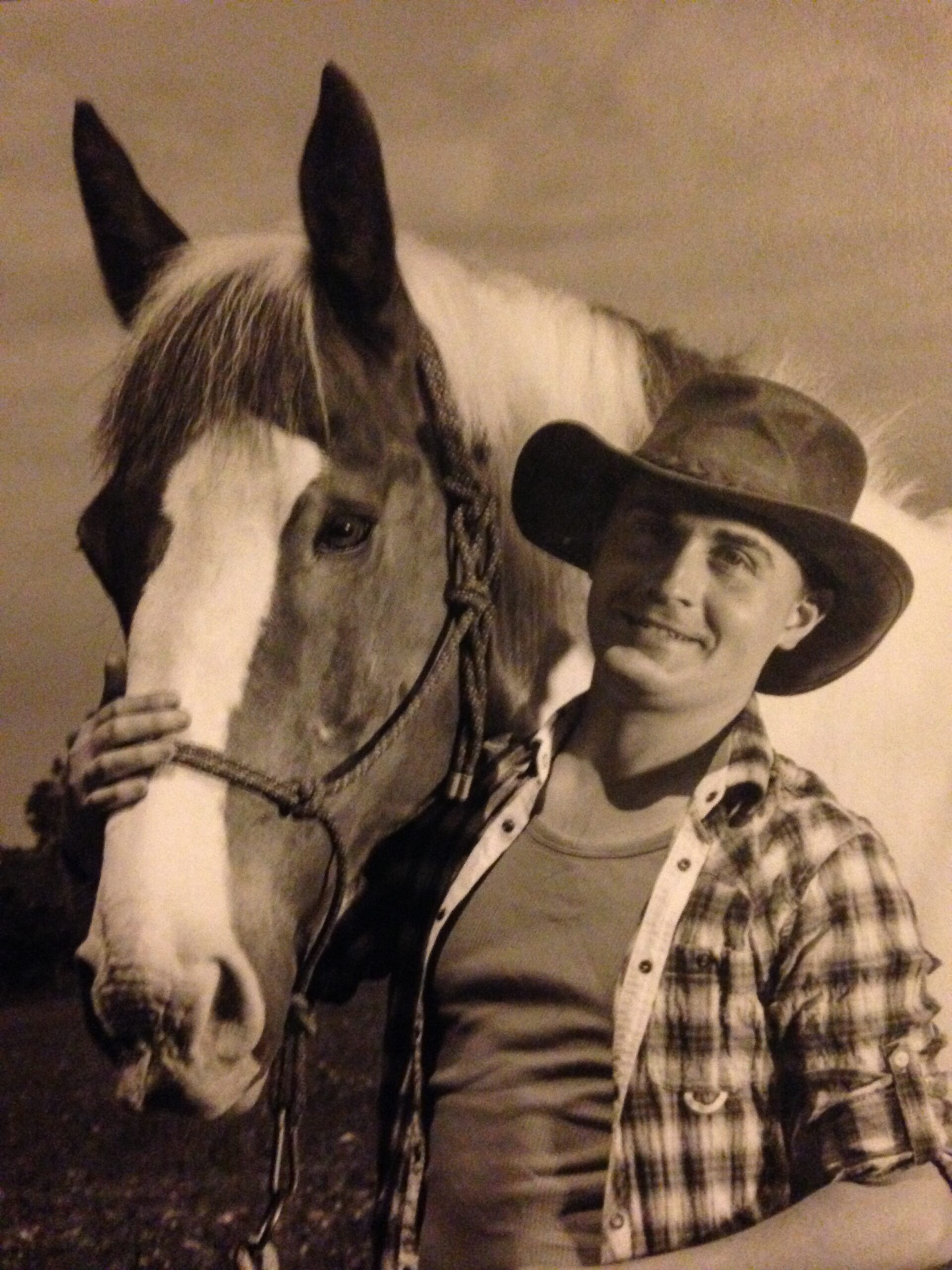
- Equine professionals with 7+ years of hands-on experience (trainers, breeders, competitive riders)
- Barn managers with an extensive animal handling background
- Professional grooms with anatomical knowledge and assessment skills
- Animal behavior specialists addressing pain-related issues
Academic Pathway:
- Graduates of animal science degree programs
- Students in veterinary or animal health programs seeking additional credentials
- Academic professionals teaching animal-related disciplines
 An animal osteopath working alongside a veterinarian, reflecting the collaborative approach central to professional animal osteopathy practice
An animal osteopath working alongside a veterinarian, reflecting the collaborative approach central to professional animal osteopathy practice
Why Professional Prerequisites Matter
The prerequisite structure serves multiple purposes:
Safety: Manual therapy techniques applied incorrectly risk injury. Professionals with existing animal handling experience understand restraint, safety protocols, and recognition of stress signals—critical for practitioner and patient safety, as explored in guides to recognizing canine communication.
Clinical Judgment: Practitioners must differentiate when manual therapy proves appropriate versus when veterinary medical intervention becomes necessary. Clinical experience develops this judgment that protects both practitioners and animals.
Foundational Knowledge: Programs build upon existing anatomical, physiological, and pathological knowledge rather than teaching these subjects from scratch. Prerequisites ensure students possess the foundation for advanced study.
Professional Integration: Successful practitioners integrate osteopathy into existing professional frameworks or practices. Prerequisites ensure students have established professional identities to which osteopathy adds value.
Credibility: The field’s professional standing depends on qualified practitioners. Prerequisites maintain standards protecting both the profession’s reputation and animal welfare.
How to Become an Animal Osteopath: Step-by-Step Pathway
The journey to animal osteopathy certification follows a structured progression through theoretical mastery, clinical skill development, and supervised practice.
Step 1: Assess Your Eligibility and Select Specialization
Self-Assessment: Evaluate your professional background against animal osteopathy requirements for the programs you’re considering. Most programs require formal qualifications in eligible categories or extensive documented experience for mature professionals.
Specialization Decision: Determine whether to pursue:
- Equine-specific certification (horses only)
- Canine-specific certification (dogs only)
- Dual certification (both species)
Specialization choice depends on your current practice focus, client base, geographic market demand, and career goals. Dual certification provides maximum flexibility but requires a longer study commitment.
Step 2: Research Animal Osteopathy Schools and Programs
When evaluating animal osteopathy schools, assess programs based on:
Accreditation and Recognition: Programs endorsed by veterinary organizations (such as American Association of Veterinary State Boards) or professional associations demonstrate established credibility. Recognition supports practice development and professional acceptance.
Faculty Expertise: Instructors should maintain active practices, demonstrating current clinical competence. Learning from practitioners who “still work in the trenches” ensures relevant, practical education rather than purely theoretical instruction.
Curriculum Comprehensiveness: Quality programs balance:
- Thorough theoretical foundations (anatomy, physiology, biomechanics, pathology)
- Systematic technical instruction (assessment and treatment protocols)
- Clinical reasoning development (when to treat, when to refer, treatment planning)
- Professional development (business practices, ethical considerations, client communication)
Practical Training Integration: Evaluate how programs ensure hands-on competency development—clinical case requirements, video assessment protocols, in-person workshops, mentorship structure.
Flexibility and Accessibility: Consider program delivery format (online, in-person, hybrid), schedule requirements, geographic location for any required attendance, and compatibility with continuing your current practice.
Graduate Support: Programs providing ongoing access to updated materials, alumni networks, and continued mentorship support long-term professional development.
Cost and Value: Tuition relative to program comprehensiveness, included materials, lifetime access provisions, and continuing education requirements.
Step 3: Complete Application and Enrollment
Application Materials typically include:
- Completed the application form with professional background details
- Credentials documentation (licenses, certificates, degrees)
- Professional resume or curriculum vitae
- Personal statement explaining motivation and career goals
- Letters of recommendation (some programs)
- Application fee (often refundable upon admission)
Processing Time: Most programs evaluate applications within days to weeks. Some conduct interviews with applicants to assess fit and readiness.
Financial Planning: Consider tuition payment options—lump sum discounts versus installment plans—and potential tax deductions for professional development education in your jurisdiction.
Step 4: Master Preclinical Theoretical Foundations
The preclinical phase establishes the knowledge base essential for clinical competence. Comprehensive programs cover:
Species-Specific Anatomy: Detailed study of skeletal structure, muscular architecture, fascial relationships, neurological pathways, and vascular supply. Equine and canine anatomy differ substantially from human anatomy, requiring thorough systematic study, as detailed in resources on horse back anatomy.
Functional Anatomy and Biomechanics: Understanding how anatomical structures produce movement, analyzing gait patterns, evaluating kinetic chains, and recognizing compensatory adaptations when dysfunction develops.
Neurophysiology: Comprehending nervous system function, pain mechanisms, proprioception, reflexive responses, and neurological integration of manual therapy interventions.
Pathology: Recognizing common conditions affecting animal patients—understanding disease processes, contraindications for manual therapy, and when veterinary referral becomes necessary. This includes conditions like canine intervertebral disc disease
Clinical Assessment Protocols: Developing systematic examination approaches—taking comprehensive case histories, performing visual and palpatory assessments, documenting findings, and developing treatment plans.
Osteopathic Philosophy and Principles: Understanding the philosophical foundations of osteopathy, principles guiding clinical decision-making, and the holistic perspective distinguishing osteopathic approaches from symptom-focused interventions.
Preclinical study typically requires 420-915 hours, depending on whether pursuing single-species or dual-species certification.
Step 5: Develop Clinical Assessment and Treatment Skills
The clinical phase translates theoretical knowledge into practical competence through systematic skill development:
Assessment Technique Development:
- Visual evaluation of posture, symmetry, gait quality, and movement patterns
- Palpation skills, identifying tissue texture changes, temperature variations, asymmetries, and restrictions
- Range of motion assessment documenting limitations and pain responses
- Integration of findings into clinical reasoning and treatment planning
Manual Technique Instruction: Learning specific interventions addressing identified dysfunctions:
- Soft tissue techniques release muscular tension and fascial restrictions
- Articular techniques improving joint mobility and function
- Strain-counterstrain approaches reduce protective muscle guarding
- Balanced ligamentous tension methods addressing chronic restrictions
- Integrated treatment approaches combining techniques systematically
Clinical Reasoning Development: Progressing beyond technical skill to clinical judgment—determining primary dysfunctions versus compensations, treatment prioritization, session planning, progression management, outcome evaluation.
Safety and Ethics: Understanding contraindications, recognizing adverse responses, maintaining professional boundaries, obtaining informed consent, documenting appropriately, and practicing within scope.
Clinical training typically requires 500-600 hours per species, involving hands-on case study completion, video submission for instructor review, and comprehensive feedback integration.
Step 6: Complete Case Studies and Final Assessment
Animal osteopathy certification requires demonstrating clinical competence through:
Clinical Case Documentation: Completing the required number of cases (typically 10-20 per species) with systematic documentation—initial assessment, treatment planning, session notes, re-evaluation, outcome measurement. Cases should demonstrate breadth across different presentations and severities.
Video Submissions: Recording complete treatment sessions showing assessment techniques, manual interventions, clinical decision-making, and professional conduct. Instructors evaluate technical precision, safety, clinical reasoning, and client communication.
Written Thesis or Research Project: Many programs require substantial written work (3,000-5,000 words) exploring a topic in depth—demonstrating research capability, critical thinking, and contribution to the professional knowledge base.
Practical Examination: Some programs require demonstrating techniques in person during intensive workshops, receiving real-time feedback and evaluation from experienced practitioners.
Step 7: Obtain Certification and Professional Designation
Upon successful program completion, graduates receive internationally recognized designations:
- Int’l DipAO: International Diploma in Animal Osteopathy (dual certification)
- Int’l DipEO: International Diploma in Equine Osteopathy
- Int’l DipCO: International Diploma in Canine Osteopathy
These credentials demonstrate completion of rigorous training meeting international standards for animal osteopathy certification.
Step 8: Consider Advanced Clinical Training
Many practitioners pursue optional intensive workshops after certification:
Masterclass Programs: Multi-day hands-on intensives providing:
- Practice on large numbers of animals (50+ dogs, 25+ horses)
- Advanced technique refinement
- Direct mentorship from experienced practitioners
- Techniques are not practical to teach online
- Peer learning and networking
While optional, these intensives significantly accelerate clinical confidence and competence through concentrated practice under expert supervision.

Animal Osteopathy Certification: Program Duration and Investment
Understanding time and financial commitments enables realistic planning for professionals considering how to become an animal osteopath.
Time Investment
Single-Species Programs:
- Canine Osteopathy: 920 hours total (approximately 12-18 months part-time)
- Preclinical: 420 hours
- Clinical: 500 hours
- Equine Osteopathy: 1,125 hours total (approximately 15-20 months part-time)
- Preclinical: 495 hours
- Clinical: 600 hours
Dual-Species Program:
- Animal Osteopathy: 2,015 hours total (approximately 24-30 months part-time)
- Preclinical: 915 hours
- Clinical Equine: 600 hours
- Clinical Canine: 500 hours
Part-time study allows professionals to maintain current practices while completing training. Full-time dedication can accelerate completion, but most students balance study with ongoing work commitments.
Practical Considerations for Career Transition
Successfully transitioning into animal osteopathy requires planning beyond educational completion.
Practice Setup and Logistics
Business Structure: Sole proprietorship, LLC, or professional corporation—each with legal, tax, and liability implications requiring professional consultation
Insurance Coverage:
- Professional liability insurance: Essential protection
- Business property insurance: Covering equipment
- Vehicle insurance: If operating a mobile practice
- Disability insurance: Protecting income capacity
Equipment and Supplies:
- Portable treatment table: $300-1,000
- Assessment tools: Goniometers, measuring devices
- Documentation systems: Electronic or paper records
- Marketing materials: Business cards, brochures, website
Regulatory Compliance:
- Business licenses and permits
- Tax registration and accounting systems
- Professional association membership
- Scope of practice understanding by jurisdiction
Marketing and Client Development
Digital Presence:
- Professional website explaining services, credentials, and approach
- Social media showcasing work (with owner permission)
- Online booking systems for client convenience
- Email marketing for existing client communication
Veterinary Relationships:
- Networking with local veterinarians, explaining a collaborative approach
- Providing educational materials about osteopathy benefits
- Maintaining professional boundaries, never diagnosing or prescribing
- Regular communication about shared clients
Community Engagement:
- Educational presentations at riding clubs, training facilities, and breed organizations
- Free assessment clinics building awareness
- Partnerships with related services (trainers, farriers, groomers)
Client Education:
- Explaining what osteopathy addresses and when it’s appropriate
- Setting realistic expectations about outcomes and timelines
- Demonstrating value through results and testimonials
- Building understanding of preventive care benefits
Continuing Professional Development
The field of animal osteopathy continues evolving through research, technique refinement, and expanding applications, as discussed in resources about the art of classical osteopathy.
Ongoing Education:
- Advanced technique workshops
- Research conference attendance
- Peer study groups and case discussions
- Cross-disciplinary learning (rehabilitation, nutrition, behavior)
Clinical Mentorship:
- Consultation with experienced practitioners on complex cases
- Peer review of treatment approaches
- Collaborative learning within professional networks
Professional Association Involvement:
- Membership in organizations like Animal Osteopathy Worldwide
- Participation in standard development
- Contribution to professional advancement
Frequently Asked Questions About Becoming an Animal Osteopath
How long does it take to become an animal osteopath?
Program completion typically requires 12-30 months, depending on specialization choice and study pace. Single-species programs (equine or canine only) require 12-20 months part-time, while dual-species certification requires 24-30 months. Full-time study can accelerate completion, though most professionals maintain current practices while studying.
Can I practice animal osteopathy without veterinary qualifications?
Yes, in most jurisdictions, animal osteopaths practice as complementary healthcare providers without veterinary licenses. However, practitioners must work within an appropriate scope—performing manual therapy techniques rather than diagnosing disease, prescribing medications, or performing surgery. Successful practitioners develop collaborative relationships with veterinarians for cases requiring medical intervention. Regulatory requirements vary by location; investigating jurisdiction-specific regulations proves essential.
What’s the difference between animal osteopathy and physiotherapy?
While both fields address musculoskeletal function, they differ in philosophical approach and technique application, as explored in resources on animal physiotherapy versus animal osteopathy. Osteopathy emphasizes whole-body assessment, identifying primary dysfunctions versus compensations, and using precise manual techniques restoring optimal biomechanics. Physiotherapy typically focuses more on rehabilitation exercises, therapeutic modalities (ultrasound, laser), and functional restoration following specific injuries. Many practitioners find the approaches complement each other effectively.
Do I need to specialize in one species?
Not necessarily. Programs offer both species-specific and dual-species certification options. Choice depends on your current practice focus and career goals. Equine specialists often work with competitive horses, while canine specialists may focus on performance dogs or rehabilitation. Dual certification provides maximum flexibility serving diverse client bases, though requires longer study commitment.
How much can I realistically earn as an animal osteopath?
An animal osteopath’s salary varies widely based on multiple factors—practice structure, location, experience, and client development. First-year practitioners typically earn $10,000-30,000 gross revenue while building clientele. Established practitioners (3-5 years) commonly achieve $40,000-80,000 gross revenue. Mature practices with strong reputations can generate $80,000-120,000+ annually. Actual net income depends on business expenses, which vary significantly between mobile and clinic-based practices.
What if I already practice human osteopathy?
Human osteopaths possess tremendous advantages transitioning to animal practice—manual skills, palpatory capabilities, clinical reasoning, and osteopathic principles transfer directly. However, quadruped anatomy, biomechanics, and handling require specific study. Animal osteopathy programs designed for healthcare professionals with manual therapy backgrounds accelerate learning by building upon existing competencies rather than teaching foundational manual skills.
Professional Education and Program Selection
For professionals committed to developing advanced skills in animal musculoskeletal assessment and treatment through classical structural osteopathy, comprehensive training from recognized institutions provides essential foundations.
The London College of Animal Osteopathy offers internationally recognized programs preparing practitioners to address complex musculoskeletal conditions through systematic manual therapy approaches rooted in thorough anatomical knowledge. Under Professor Stuart McGregor’s personal mentorship—who pioneered animal osteopathy over 40 years ago—practitioners learn:
- Comprehensive species-specific anatomy and biomechanics
- Systematic clinical assessment protocols
- Precise manual therapy techniques
- Clinical reasoning distinguishing primary dysfunction from compensation
- Professional practice development and ethical considerations
- Integration within veterinary-collaborative care models
LCAO’s programs serve the diverse professional backgrounds eligible for animal osteopathy training—from veterinarians expanding treatment capabilities to manual therapists transitioning into animal healthcare to experienced animal professionals seeking formal credentials.
With 1,600 graduates across 72 countries, LCAO has established the educational standards for animal osteopathy certification internationally. The flexible online format with comprehensive clinical mentorship enables professionals worldwide to access rigorous training without relocating or abandoning current practices.
Conclusion
The pathway to becoming an animal osteopath rewards professionals with established animal health or manual therapy backgrounds who seek to expand their capabilities through advanced manual therapy training. Understanding animal osteopathy requirements—both formal prerequisites and personal attributes—enables a realistic assessment of fit with this specialized field.
Animal osteopathy certification through comprehensive programs provides the theoretical knowledge, technical skills, clinical reasoning, and professional preparation necessary for confident independent practice. While animal osteopath salary and earning potential vary based on numerous factors, most practitioners find the field financially sustainable while offering profound professional satisfaction through meaningful impact on animal welfare and performance.
For those exploring animal osteopathy schools and programs, prioritizing accredited education from recognized institutions, comprehensive curricula balancing theory and practice, experienced faculty maintaining active clinical practices, and flexible delivery enabling continued professional practice ensures optimal preparation for successful careers.
The investment—whether measured in time, finances, or professional risk—yields returns through expanded career opportunities, enhanced professional capabilities, deeper understanding of animal biomechanics and function, and the satisfaction inherent in helping animals achieve optimal musculoskeletal health and comfort.
Whether you bring veterinary expertise, manual therapy skills, animal healthcare experience, or dedicated hands-on practice with horses or dogs, the path to animal osteopathy certification offers structured progression toward a profession combining intellectual challenge, technical skill, animal connection, and meaningful contribution to animal healthcare.