The Importance of Saddle Fit for Horses: Ensuring Comfort and Performance
The Importance of Saddle Fit for Horses: Ensuring Comfort and Performance
By Siun Griffin, Equine Physiotherapist and LCAO Community Manager
A well-fitting saddle is crucial for the overall well-being, comfort, and performance of horses. It plays a pivotal role in maintaining the horse’s physical and mental health.
Here, we will delve into why saddle fit is so important, provide basic checks horse owners can perform, discuss factors affecting saddle fit, and highlight the positive and negative effects of a well-fitting and poorly fitting saddle on the horse’s body, movement, and behavior.
Why Saddle Fit Matters
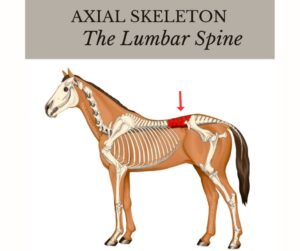
A properly fitting saddle allows the horse to move freely, without restrictions or discomfort. It distributes the rider’s weight evenly across the horse’s back, minimizing pressure points and avoiding potential injuries. A well-fitting saddle also enhances communication between horse and rider, promoting trust and cooperation.
Basic Saddle Fit Checks
Horse owners can perform a few simple checks to evaluate saddle fit.
1. Wither Clearance
Adequate wither clearance is crucial to prevent pressure on the sensitive withers. To check, run your hand under the pommel of the saddle while it is on the horse’s back. There should be enough space to comfortably slide a few fingers (about 3) between the withers and the saddle. Insufficient clearance can lead to discomfort and restricted shoulder movement.
2. Length of the Saddle
The saddle’s length should match the horse’s back appropriately. To assess this, place the saddle on the horse without a pad and ensure that the saddle panels are in contact with the back along their entire length. Check that the cantle (rear part of the saddle) does not extend beyond the horse’s last rib.
3. Balance and Stability
When the saddle is correctly placed, it should sit evenly and securely on the horse’s back. It should not rock or tilt forward or backward. Observe the saddle from various angles to ensure it maintains stability during movement. A balanced saddle contributes to the horse’s overall comfort and helps the rider maintain proper position and balance.
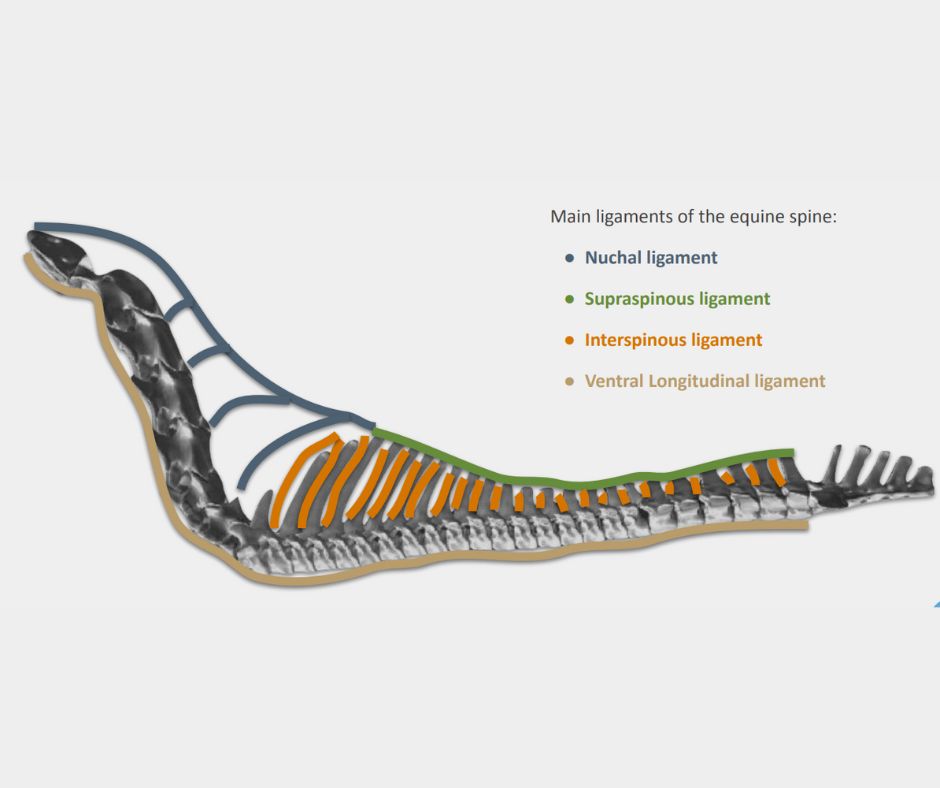
4. Gullet Clearance
The saddle’s gullet, located underneath the pommel, should provide sufficient clearance for the horse’s spine. Press gently along the gullet while the saddle is on the horse’s back to confirm that it is not touching or exerting pressure on the spine. Proper gullet clearance is vital to prevent discomfort and potential back problems.
5. Panel Contact
The saddle’s panels, which rest on the horse’s back, should have even contact and distribute the rider’s weight uniformly. Look for consistent panel contact without any noticeable gaps or pressure points.
Remember, these basic checks provide a starting point for assessing saddle fit. While they can give you a good idea of if a saddle will be suitable, it is best to get a professional fitter to evaluate as well.
A professional saddle fitter or an experienced equestrian can assess the saddle fit with expertise and take into account the unique characteristics of both horse and rider.
A horse will change shape over the year, which can affect the saddle fit. By conducting regular saddle fit checks and ensuring the saddle meets the horse’s requirements, we can contribute to the horse’s well-being, comfort, and overall performance.
Factors Affecting Saddle Fit
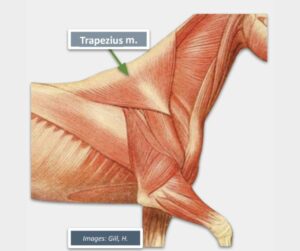
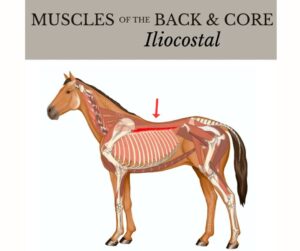
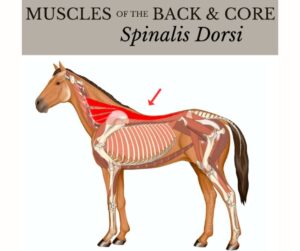
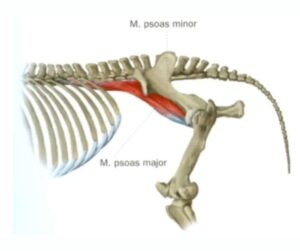
Several factors influence saddle fit. The horse’s conformation, age, and musculature can all impact the suitability of a saddle.
The rider’s weight, riding discipline, and personal preferences also play a role. Furthermore, the type of saddle, such as dressage, jumping, or western, must be appropriate for the intended use.
Positive Effects of a Well-Fitting Saddle
A well-fitting saddle offers numerous benefits to the horse. Firstly, it enables unrestricted movement, allowing the horse to engage its back, shoulder, and hindquarters effectively.
This contributes to improved balance, suppleness, and overall athleticism. Secondly, a comfortable saddle prevents discomfort, pain, and the development of sore spots, ultimately preserving the horse’s physical well-being and performance capabilities.
Lastly, a well-fitted saddle promotes relaxation and positive behavior, leading to a harmonious partnership between horse and rider.
Negative Effects of a Poorly Fitting Saddle
Using an ill-fitting saddle can have severe consequences for the horse. It can lead to discomfort, pain, and even long-term physical damage.
Pressure points caused by an improperly fitted saddle can result in muscle atrophy, bruising, and soreness. Over time, this may lead to behavioral issues such as resistance, unwillingness to work, and even aggression.
Poor saddle fit can also cause gait abnormalities, stiffness, and reduced performance potential.
Final Thoughts
Investing time and effort into ensuring proper saddle fit is essential for every responsible horse owner.
By performing regular saddle fit checks, seeking professional guidance when necessary, and choosing saddles that suit the horse’s conformation and riding discipline, we can safeguard our equine partners’ well-being, comfort, and performance.
A well-fitting saddle allows horses to move freely, helps prevent injuries, and nurtures a positive relationship between horse and rider. Let us prioritize the welfare of our horses by recognizing the significance of saddle fit in their lives.
Saddles are expensive. However, it is best not to buy cheaper models new or used. This will cost you more in the long run and physically and mentally damage your horse. It is always better to look for a quality brand. When well maintained a quality saddle will last you years.
(Note: This article is for informational purposes only. For detailed advice on saddle fit, please consult a professional saddle fitter or an experienced equestrian.)
For more information on how you can become an Equine Osteopath, click here