Hip Dysplasia in Dogs: Natural Treatment Guide
Understanding Hip Dysplasia in Dogs
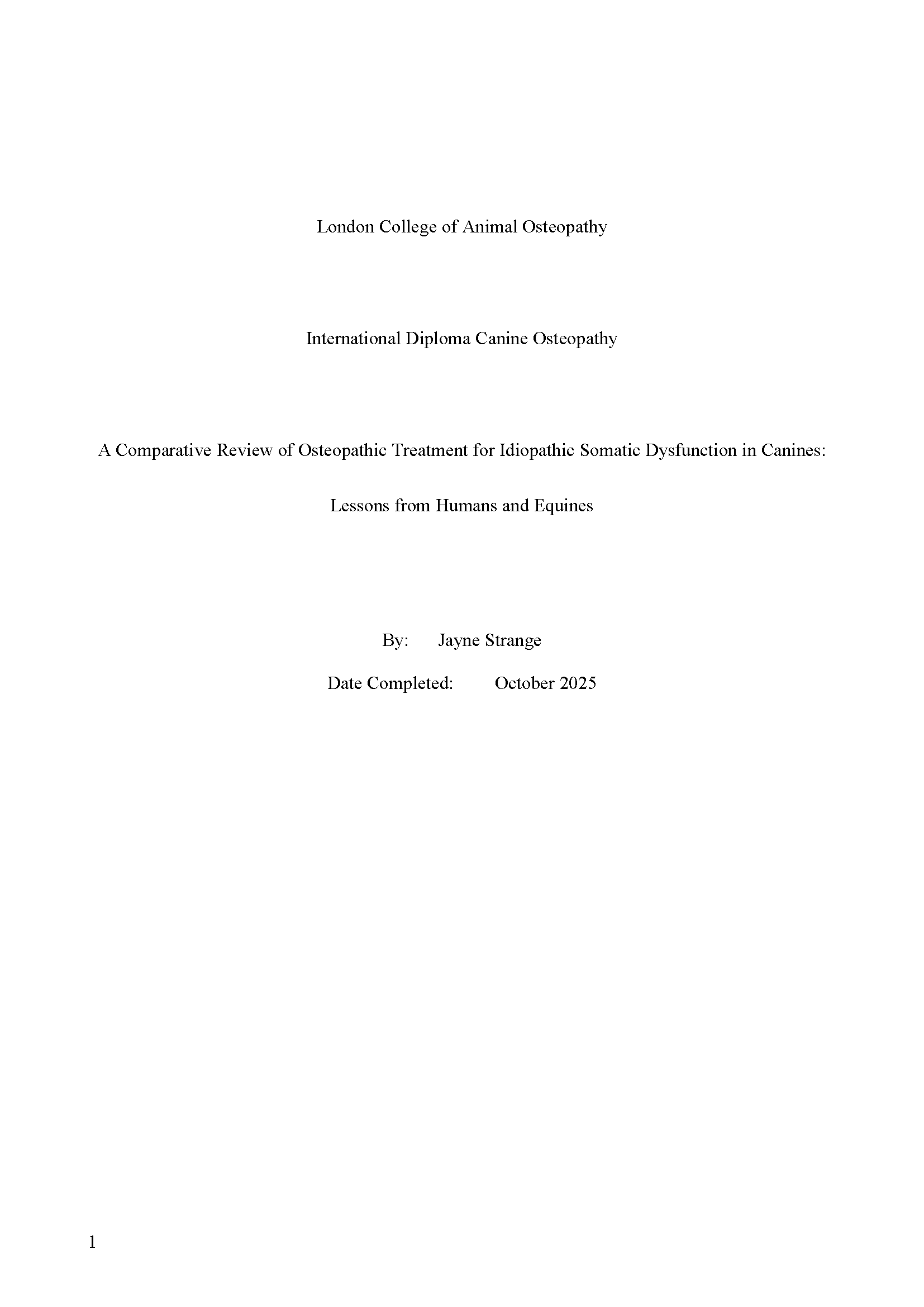
Hip dysplasia in dogs (often called CHD, or canine hip dysplasia) is a developmental joint condition in which the femoral head and the acetabulum don’t form a stable, congruent ball-and-socket joint. Over time, that laxity causes abnormal wear, inflammation, and osteoarthritis. Clinical signs range from subtle exercise intolerance to obvious lameness. Early identification and a tailored plan make the biggest difference to long-term comfort and mobility.
Signs to Watch For
- Stiffness, especially after rest
- “Bunny-hopping” gait
- Reluctance to climb stairs or jump
- Muscle loss in the hind limbs
- Difficulty getting up
Early diagnosis is vital. Vets use physical exams, gait assessment, and imaging (X-rays or CT) to confirm the condition.
What Natural Treatment for Hip Dysplasia Really Means
When owners ask about natural treatment for hip dysplasia, they usually mean therapies that reduce or avoid invasive surgery and focus on restoring comfort and mobility through conservative care. For many dogs — particularly those with mild laxity or early osteoarthritis — a multimodal, natural approach can maintain function and reduce pain for years.
It’s important to remember that these treatments don’t fix the joint structure. Instead, they manage inflammation, support muscle strength, and help slow the degenerative process.
Weight and Nutrition: The Foundation of Every Plan
Excess weight is one of the most significant risk factors in hip dysplasia treatment in dogs. Extra load accelerates cartilage wear and increases inflammation. Keeping your dog lean is essential.
- Maintain an ideal body condition score — you should be able to feel ribs but not see them.
- Use a balanced, veterinary-approved diet that supports joint and muscle health.
- Include anti-inflammatory nutrients such as omega-3 fatty acids (EPA/DHA), which have strong evidence for reducing joint inflammation.
Exercise and Rehabilitation for Hip Dysplasia Without Surgery
For many dogs, hip dysplasia without surgery can be managed successfully through structured exercise and rehabilitation. Controlled, low-impact movement helps strengthen the muscles that stabilise the hip joint.
- Avoid repetitive jumping, sprinting, or rough play on hard surfaces.
- Focus on regular leash walks, gentle inclines, and hydrotherapy.
- Underwater treadmill therapy is particularly effective for maintaining muscle tone without overloading the hips.
A tailored rehabilitation plan — developed by a veterinary physiotherapist or canine rehabilitation specialist — can dramatically improve comfort and movement.
When Non-Surgical Treatment Works Best
- Dogs with mild to moderate joint laxity
- Puppies showing early signs
- Older dogs who are poor surgical candidates
Veterinary management often includes:
- Weight control to reduce joint load
- Anti-inflammatory medication
- Joint supplements (e.g., omega-3 fatty acids, glucosamine)
- Controlled exercise and hydrotherapy
Pain Management and Supportive Therapies
“Natural” care doesn’t mean avoiding all medication. NSAIDs prescribed by your veterinarian remain key tools in controlling inflammation and pain when needed. The goal of canine hip dysplasia natural treatment is to reduce long-term drug reliance by combining medication with other therapies — not to exclude medical management entirely.
Other adjunctive options include:
- Laser therapy and acupuncture: which may improve pain control.
- Shockwave or ultrasound therapy: used in some veterinary rehab settings to support healing.
- Therapeutic exercise and stretching: which maintain flexibility and prevent compensatory strain.
Supplements and Diet Adjustments
Diet plays a central role in managing hip dysplasia. Overnutrition during growth can worsen joint instability, while certain nutrients support joint health.
- Omega-3 fatty acids from marine sources have the strongest veterinary evidence for joint support.
- Glucosamine and chondroitin show mixed but promising results in maintaining cartilage health.
- Green-lipped mussel extract and curcumin are being studied for their anti-inflammatory effects.
Always consult your vet before starting supplements, especially if your dog is on other medications.
Puppy Hip Dysplasia: Early Screening and Prevention
Puppy hip dysplasia can develop silently during growth. Early screening for hip laxity in large or at-risk breeds can guide prevention. While some surgical procedures (like juvenile pubic symphysiodesis) can alter hip development, conservative care is also vital.
- Feed an appropriate large-breed puppy diet to control growth rate.
- Avoid over-exercising growing pups.
- Keep puppies lean — rapid growth and excess weight increase risk.
Early management gives the best chance of long-term joint stability and comfort.
Risk Factors and Genetics
Puppies from predisposed breeds should be monitored closely. Responsible breeding, hip scoring, and balanced diets during growth are essential.
Safe Growth and Exercise
Avoid overfeeding or excessive exercise during rapid growth phases. Controlled movement on non-slip surfaces supports healthy joint development.
Early Intervention
If detected early, supportive care — including physiotherapy, targeted nutrition, and monitored activity — can reduce severity later in life.
Canine Osteopathy: What It Can and Cannot Do
Canine osteopathy is a gentle, manual therapy that can help reduce muscle tension, improve local mobility, and relieve compensatory strain caused by hip instability. When used appropriately, it complements veterinary and rehabilitation care.
When Osteopathy Can Help:
- Improving soft-tissue flexibility around the hip
- Improving comfort and range of motion
- Supporting overall body balance during recovery
When Osteopathy Should Not Be Used:
- Correct bone deformity or joint laxity
- Replace surgical or veterinary medical treatment when required
- The best results come from an integrated approach, where osteopathy supports physiotherapy, hydrotherapy, and veterinary management as part of a complete plan.
Practical Checklist for Owners
- Confirm diagnosis through veterinary imaging (X-rays, PennHIP, or OFA screening)
- Maintain a lean body weight and balanced nutrition
- Combine rehabilitation, osteopathy, and exercise therapy
- Discuss appropriate supplements with your vet
- Schedule regular follow-ups to adjust the plan as your dog’s needs change
Long-Term Outlook and Multidisciplinary Care
Successful management of canine hip dysplasia relies on a team approach: vets, osteopaths, physiotherapists, hydrotherapists, and owners working together.
A tailored plan can maintain comfort and mobility for years — even without surgery — provided that inflammation is managed and weight is controlled.Q&A: Common Questions About Hip Dysplasia in Dogs
Q: Can hip dysplasia in dogs be treated without surgery?
Yes. Mild to moderate cases often respond well to non-surgical management, including weight control, physical rehabilitation, and nutritional support. This approach manages pain and function but does not change joint structure.
Q: What are the best natural treatments for canine hip dysplasia?
A combination of omega-3 fatty acids, structured exercise, hydrotherapy, osteopathy, and physiotherapy can help. Always base your plan on veterinary advice.
Q: Can puppy hip dysplasia be prevented naturally?
You can reduce risk through balanced nutrition, controlled growth, and safe exercise — but genetics still play a major role. Early veterinary screening remains essential.
Enrichment Activities for Dogs: Supporting Physical and Neurological Health
Canine enrichment has evolved far beyond the notion of entertainment. For the educated practitioner, enrichment is understood as a cornerstone of both physical and neurological health.
Dogs, as sentient, highly adaptable beings, require more than food and shelter to thrive. They need structured activities that challenge their cognitive abilities, engage their sensory systems, and maintain musculoskeletal balance. When viewed through the lens of osteopathy, enrichment plays a crucial role in sustaining functional integrity and preventing compensatory strain.
Why Enrichment Matters Beyond Behaviour
Enrichment is often marketed as a behavioural solution for boredom or anxiety, but its benefits extend far deeper. Physical inactivity contributes not only to behavioural problems but also to functional restrictions in fascia, muscles, and joints. Lack of movement diversity can result in asymmetrical loading patterns, reduced range of motion, and subsequent compensatory chains. From an osteopathic perspective, this predisposes tissues to dysfunction and discomfort long before clinical pathology emerges.
Conversely, enrichment activities such as scent games, proprioceptive exercises, and structured play introduce variability in movement and stimulate the body’s adaptive mechanisms. They provide controlled stressors that encourage neuromuscular responsiveness and maintain elasticity in connective tissue—a key principle in sustaining health.
Types of Enrichment and Their Osteopathic Relevance
- Sensory and Cognitive Games
Scent-based activities, such as tracking or nose work, activate neural pathways linked to olfaction, but they also demand postural adjustments and dynamic balance as the dog moves through varied terrain. These micro-adjustments stimulate joint proprioceptors and promote fluid motion, supporting the osteopathic principle that structure and function are interdependent. - Proprioceptive Challenges
Exercises involving unstable surfaces, balance discs, or low obstacles engage the deep stabilising musculature and improve coordination. For an osteopath, these activities are particularly relevant because they help maintain joint congruency and reduce compensatory strain. Proprioceptive enrichment aligns with preventative care, limiting the risk of dysfunction that may later require manual intervention. - Environmental Interaction
Allowing dogs to explore varied surfaces such as, sand, grass, and gravel, not only satisfies their sensory curiosity but also creates differential loading patterns in the musculoskeletal system. Such variation supports tissue adaptability, reducing the likelihood of repetitive strain and fascial restriction.
Enrichment as a Complement to Osteopathic Care
When osteopaths work with dogs presenting with musculoskeletal discomfort, restricted motion, or compensatory patterns, treatment does not end on the table. Integrating appropriate enrichment activities into a care plan extends the therapeutic effect by encouraging active participation in recovery.
For example, controlled proprioceptive exercises post-treatment can help re-establish neuromuscular control and reinforce balanced posture. Similarly, gentle cognitive games can reduce stress hormones, improving systemic health and tissue healing capacity.
Enrichment also serves as a preventative strategy. Osteopaths often encounter functional restrictions resulting from monotonous activity patterns – urban dogs walking the same flat routes daily, or working dogs repeatedly performing specific motions. A structured enrichment program disrupts these patterns, introducing variability that sustains adaptability in joints, fascia, and neurology.
A Holistic View of Canine Health
The osteopathic model emphasises the unity of body, mind, and environment. Enrichment embodies this philosophy by engaging the dog as a whole – stimulating the nervous system, supporting biomechanical integrity, and satisfying behavioural needs. For the well-informed canine professional, enrichment is not a luxury but a therapeutic and preventative necessity. When integrated thoughtfully, it becomes an extension of osteopathic care, maintaining the functional harmony that defines true health.
Stay tuned for Parts 2 and 3 in this series.
Cranky or Crooked? When ‘Grumpy’ Pets Might Need a Physical MOT
We often think of a pet’s bad mood as a behavioural problem. A dog growls more than usual, a horse pins its ears when being tacked up, or a normally affectionate cat hides under the bed. While temperament certainly plays a role in how animals interact with the world, sudden changes in mood or willingness can be an early warning sign of physical discomfort.
Behaviour as the Body’s Messenger
Animals cannot tell us directly when something hurts, so behaviour becomes their first language of discomfort. Withdrawal, irritability, or avoidance of handling can all be subtle signals. In many cases, these behaviours develop gradually, making them easy to dismiss as “getting older” or “being stubborn.” However, pain, particularly musculoskeletal pain, can subtly shift the way an animal moves, rests, or tolerates certain interactions, and those changes often affect mood.
From Spine to Stifle: Common Physical Causes
A stiff neck, sore back, joint inflammation, or muscle strain can all contribute to an animal’s grumpiness. Dogs with early hip dysplasia may be less willing to jump into the car. Horses with sacroiliac discomfort may buck or resist collection under saddle. Even seemingly minor issues, such as low-grade tendon strain, can have an outsized effect on behaviour, because animals are masters at compensating physically until discomfort becomes significant enough to alter their mood.
The Role of a Physical MOT
A “physical MOT” for animals works much like a routine service check for a car: it identifies early signs of wear, misalignment, or strain before they lead to bigger problems. This assessment might involve veterinary examination, gait analysis, palpation of muscles and joints, and review of recent performance or activity changes. The aim is not just to find an obvious injury but to pick up on the small, chronic issues that can gradually chip away at comfort and, by extension, behaviour.
When to Take Action
Changes in mood that last more than a few days, especially when paired with changes in movement or posture, warrant further investigation. Repeated avoidance behaviours, like resisting grooming, pulling away from certain touch, or becoming more vocal during routine handling, can be the body’s equivalent of a “warning light.” Early assessment and intervention often mean faster recovery, less pain, and a return to the pet’s usual, more agreeable self.
Balancing Behaviour and Physical Care
Not every grumpy moment signals pain, but it’s equally unwise to assume it’s “just personality” without ruling out physical causes. In many cases, addressing underlying discomfort improves not only performance but also the bond between animal and handler. By combining behavioural awareness with regular physical check-ups, owners can ensure they’re not just managing a mood, they’re supporting an animal’s overall wellbeing.
Not Just a Hose Job: The Right Way to Cool Dogs and Horses in Hot Weather
Some myths are hard to kill. Every summer, they resurface, usually in Facebook threads with 150 comments and rising tension.
“Never hose a horse’s back!”
“Don’t pour water on dogs; it traps the heat!”
You’ve probably seen it. Maybe even argued it. So let’s cut through the noise and get down to what actually works, what doesn’t, and when the stakes are high enough to call the vet.
First: Heat Kills, Fast
Hyperthermia isn’t a vague risk. It’s a medical emergency. In dogs, a body temperature above 39.5°C (103.1°F) is considered abnormal, and above 41°C (105.8°F) is classified as heatstroke, with a high risk of organ damage, coagulopathies, and CNS dysfunction (1)(2).
Horses follow a similar pattern. Heatstroke is generally diagnosed when body temperatures exceed 41.5°C (106.7°F), with neurological signs and cellular injury likely to follow soon after (3).
So no, this isn’t just about comfort.
Signs You’re in Trouble
Whether it’s a dog or a horse, these are red flags:
- Rapid, shallow breathing
- Bright red (or very pale) gums
- Weakness, wobbliness, or collapse
- Vomiting (dogs), diarrhea (sometimes bloody)
- Seizures or confusion
- No longer sweating (in horses) despite high effort
- Red gums/tongue (dogs & cats)
- Panting (dogs & cats)
- Drooling (dogs & cats) (9)
- Collapse
If you’re seeing these? This is not the time to “let them rest in the shade” and reassess later. Call a vet immediately. Start cooling while you wait.
Cool Fast, Cool Properly
Let’s talk methods. Because yes, how you cool matters, but probably not in the way you’ve heard.
Horses: The Continuous Cold Water Debate
Here’s the short version: hosing is good. Repeated hosing with cold water is better. Scraping? Optional. And no, cold water doesn’t cause shock.
A number of studies have confirmed what we now know works: cold water applied continuously and repeatedly is one of the most effective ways to lower core body temperature in horses after exercise in hot conditions (4)(8). And no, you don’t have to avoid the large muscles or scrape between rounds. In fact, scraping actually slows the cooling process.
What to do:
- Move the horse into the shade
- Hose cold water over the entire body
- Repeat continuously until rectal temp drops below 38.5°C
- Use fans if you have them
Stop scraping. It’s not doing what you think it is. Scraping was useful when water was scarce or hot; today, it just slows you down.
Dogs: Water Is Not the Enemy
The claim that water “traps heat” on dogs? It’s a misinterpretation of evaporative cooling. Sure, if you pour water on and leave it without airflow, it won’t help much. But if you’re using cold water and creating airflow (with a fan, breeze, or toweling), it’s effective (5).
What to do:
- Get them into shade or air con
- Soak with cool water: belly, armpits, paws
- Use a fan or breeze to promote evaporation
- Offer water to drink (but don’t force it)
- If temp >40°C (104°F), get to a vet now
- Cool water immersion if the dog is otherwise young and healthy (9)
- Hosing with cool water (ensure it is running cool before applying)
Don’t wrap them in wet towels. That insulates heat unless you repeatedly change them. Other methods, such as those listed above, are more effective. And don’t wait for panting to “settle”; panting alone doesn’t cool enough in high humidity. If in any doubt, call your vet immediately as further intervention may be necessary.
Common Myths (And Why They Stick Around)
Some of these beliefs have been around for decades. Let’s unpack a few:
“Cold water causes shock.”
This comes from confusion with immersion shock in humans. Animals don’t respond the same way. Gradual cooling doesn’t increase the risk of shock; it reduces the risk of organ damage.
“Scraping water is essential.”
Only if you’ve got gallons of hot water and no breeze, otherwise, keep spraying (4).
“Cooling must be slow.”
Nope. Rapid cooling saves lives. Delays kill (1)(4).
Other Factors That Raise Risk
Even well-cared-for animals can overheat. But some are more at risk:
- Brachycephalic breeds (Pugs, Frenchies, Bulldogs)
- Horses with anhidrosis (poor/no sweating)
- Obese or heavily muscled animals
- Thick-coated breeds in humid weather
- Older or chronically ill animals
And don’t forget: if they’ve overheated once, they’re more vulnerable next time. Heatstroke causes cumulative damage.
Final Thoughts: Don’t Wait to Be Sure
By the time you’re sure it’s heatstroke, you’re probably already late. When in doubt, cool and call. You won’t regret being wrong, but you will regret being too late.
Resources
1. VCA Animal Hospitals. Heat Stroke in Dogs. https://vcahospitals.com/know-your-pet/heat-stroke-in-dogs
2. Pathophysiology of heatstroke in dogs – revisited. PMC, 2018. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5800390/
3. Marlin, D.J., & Nankervis, K. (2002). Equine Exercise Physiology. Wiley-Blackwell. Summarised in: AAEP Guidelines on Heat Stress: https://aaep.org/horsehealth/heat-stress-horses
4. Marlin, D.J., Scott, C.M., Roberts, C.A., Casas, I., Holah, G., & Schroter, R.C. (1998). Post exercise cooling strategies in hot, humid conditions. Equine Veterinary Journal, 30(S27), 337–340. https://doi.org/10.1111/j.2042-3306.1998.tb04426.x
5. ACVIM / VETgirl. How to Treat Heatstroke in Dogs. VetGirl Veterinary Continuing Education blog. “Heatstroke is defined as a non‑pyrogenic elevation in core body temperature greater than 105.8 °F (41 °C) along with central nervous system dysfunction.” https://vetgirlontherun.com/how-to-treat-heastroke-in-dogs-vetgirl-veterinary-continuing-education-blog/
6. Veterinary Voices UK. Cool, Icy, Cold or Tepid? What’s Best for Heat Stroke? Myth‑Busting blog post, June 26, 2024. “Pour, hose or if possible immerse the pet in very cold water… Do not drape in towels and leave them in situ.” https://www.vetvoices.co.uk/post/cool-icy-cold-or-tepid
7. VetCompass UK – Heat-Related Illness in Dogs: Risk Factors and Clinical Signs. https://www.vetcompass.org/media/1312/heat-related-illness-dogs.pdf
8.Vet Times (2022). Don’t be afraid of the hosepipe – cold water won’t cause shock in horses. https://www.vettimes.co.uk/news/dont-be-afraid-of-the-hosepipe-cold-water-wont-cause-shock-in-horses/
9. Royal Veterinary College (RVC). Heatstroke in Dogs and Cats: Fact File. Royal Veterinary College Small Animal Department. “Dogs and cats can suffer from heatstroke, a life-threatening condition where the body temperature increases … organ failure and even death can occur.” https://www.rvc.ac.uk/small‑animal‑vet/teaching‑and‑research/fact‑files/heatstroke‑in‑dogs‑and‑cats
Beyond the Hips and Elbows: Atypical Presentations of Osteoarthritis in Dogs
When we think about osteoarthritis (OA) in dogs, our minds often jump straight to the hips and elbows, and with good reason. These are the most commonly affected joints, particularly in breeds predisposed to hip or elbow dysplasia. But OA doesn’t always follow the “classic” patterns. In fact, it can show up in far less obvious places, quietly affecting a dog’s comfort, mobility, and quality of life in ways that are easy to miss if we’re not looking for them.
Let’s take a closer look at the less-talked-about joints, the carpus, hock, digits, and even the spine, and explore how these atypical presentations can subtly change a dog’s movement, behavior, and day-to-day function.
Why Atypical OA Matters
Osteoarthritis is a degenerative joint disease characterised by cartilage breakdown, synovial inflammation, osteophyte formation, and changes in subchondral bone [1]. While large, weight-bearing joints are most often discussed, any synovial joint in the body can be affected. Atypical sites are often overlooked in general practice, especially when signs are mild or masked by compensation.
Carpal OA: The Silent Stiffness
The carpus is vital for shock absorption and flexion during locomotion. Arthritis in this joint may not cause overt lameness early on, but signs may include:
- Reluctance to jump or go downstairs
- Reduced range of motion in flexion
- Stiffness after rest
- Flattening or “pancaking” of the paw during stance
Radiographic evidence of carpal OA is relatively uncommon compared to hips or elbows, but it does occur, particularly in working dogs or those with a history of repetitive strain or trauma [2].
Hock OA: A Subtle Hind-End Saboteur
The tarsus (hock) is another joint that gets little attention until something goes wrong. Dogs with hock OA may show:
- Abnormal limb carriage (e.g., toe-touching or inward rotation)
- Difficulty navigating uneven terrain
- Decreased propulsion when running or climbing
- Overdevelopment of compensatory muscles in the lumbar or gluteal region
Hock OA can result from chronic instability, as seen in shelties or collies with tarsal injuries, or post-traumatic arthritis in active breeds [3].
Digits: When the Toes Take the Hit
The interphalangeal joints are small, but they bear significant force with each step. Toe OA often flies under the radar because:
- Dogs may simply appear “off” without clear lameness
- Owners may report vague signs like “slowing down”
- It’s often dismissed as age-related stiffness
Toe OA is particularly common in large breeds, senior dogs, or those with past ligamentous injuries. One study found interphalangeal OA in 13% of dogs undergoing full-body radiographs for unrelated conditions [4].
Axial Joints: Spine and Sacroiliac Involvement
Though technically distinct from appendicular OA, degenerative changes in the spine, including spondylosis deformans and facet joint OA, are increasingly recognised in ageing dogs. These changes can:
- Mimic hip OA symptoms
- Cause reluctance to jump or twist
- Lead to compensatory overload in thoracic limbs
Advanced imaging (CT/MRI) is often required to accurately assess these changes, but clinical suspicion should be high in dogs with back pain, hindlimb weakness, or poor response to traditional OA therapies [5].
Clinical Relevance: What to Watch For
In atypical OA, behavioral and functional changes are often more telling than overt lameness. Watch for:
- Shifting weight or frequent postural changes
- Persistent licking or chewing at a limb
- Avoidance of certain movements (e.g., digging, sharp turns)
- Reduced performance in working or sporting dogs
Gait analysis, palpation, and range-of-motion testing are essential to pick up subtle deficits. Diagnostic imaging can confirm, but shouldn’t replace clinical insight.
A Multimodal Mindset
Management of atypical OA is similar to classic OA but may require more targeted strategies:
- Manual therapies (osteopathy, physio, massage) can improve joint mobility and reduce compensatory strain.
- Low-impact exercise like underwater treadmill therapy helps maintain function without overload.
- NSAIDs, gabapentin, and disease-modifying osteoarthritis drugs (DMOADs) are often used pharmacologically.
- Weight management remains critical, especially for distal limb and spinal OA [6].
Final Thoughts
Osteoarthritis in dogs is not always where you expect it, and that’s exactly why we need to stay curious. By widening our clinical lens beyond the hips and elbows, we can catch the quieter forms of OA early and intervene with strategies that truly make a difference.
References
- Johnston, S. A. (1997). Osteoarthritis. Joint anatomy, physiology, pathobiology, and basic treatment principles. Veterinary Clinics of North America: Small Animal Practice, 27(4), 699–723. https://doi.org/10.1016/S0195-5616(97)50075-3
- Paster, E. R., & Bristol, D. G. (2003). Carpal and Tarsal Joint Disease in Dogs. Compendium on Continuing Education for the Practicing Veterinarian, 25(2), 110–122.
- Kapatkin, A. S., et al. (2002). Tarsal osteoarthritis: A retrospective study. Veterinary Surgery, 31(2), 127–132. https://doi.org/10.1053/jvet.2002.31763
- Morgan, J. P., et al. (1968). Skeletal dysplasias and arthropathies in the dog. Veterinary Radiology, 9(4), 122–131.
- Dewey, C. W., & da Costa, R. C. (2015). Practical Guide to Canine and Feline Neurology. Wiley-Blackwell.
- Moreau, M., et al. (2010). Clinical evaluation of a nutraceutical, carprofen and meloxicam for the treatment of dogs with osteoarthritis. Veterinary Record, 166(3), 72–77. https://doi.org/10.1136/vr.b4713
Bringing Bodywork to the Boroughs: Urban Osteopathy and Holistic Therapies for Pets
In the bustling heart of the city, amid high-rises, traffic, and concrete, an unexpected movement is quietly gaining momentum: the rise of animal osteopathy and holistic therapies in urban environments. Once considered niche or rural, these hands-on approaches are proving essential for city-dwelling animals coping with the unique physical and emotional demands of urban life.
Urban Pets, Urban Problems
Unlike their countryside counterparts, urban animals, particularly dogs and cats, face daily challenges that can subtly wear on their musculoskeletal systems and emotional well-being. Slick floors, tight spaces, long hours alone, limited green areas, and overstimulation from noise and crowds are just a few of the factors that can contribute to compensatory movement patterns, chronic tension, behavioural reactivity, or even injury.
For city animals, especially those confined to apartments or on-lead for most of their day, the opportunity for natural movement is restricted. This lack of freedom to stretch, climb, run, or play off-lead can lead to muscular imbalances, joint stiffness, and emotional frustration. These issues are often invisible to owners until pain, mobility problems, or behaviour changes arise.
The Role of Osteopathy in the City
Animal osteopathy offers a gentle, holistic way to address the effects of urban living. Using hands-on techniques such as myofascial release, joint mobilisations, and craniosacral work, osteopaths support the animal’s body in restoring alignment, releasing tension, and improving function. Importantly, osteopaths consider the whole animal, not just the site of pain or injury.
In an urban context, this full-body approach is particularly valuable. A dog with shoulder strain from pulling on the lead may also have compensatory tension through the back and pelvis. A cat that slips repeatedly on smooth wooden floors may develop stiffness or altered posture. In both cases, osteopathy addresses not only the biomechanical problem but also how the nervous system and environment contribute.
Home Visits and Adaptability
One of the unique aspects of urban practice is the need for adaptability. Many animal osteopaths and holistic therapists in cities provide home visits, a practical necessity in areas where clinic space is limited or non-existent. While this approach removes the stress of travel for the animal, it presents its own challenges: narrow hallways, limited floor space for movement assessments, stairs instead of lifts, and curious household distractions.
Still, therapists learn to improvise, using yoga mats for grip, adapting exercises to stairwells or hallways, and teaching owners how to support their animal’s well-being with small, consistent changes at home.
Working Collaboratively in a Crowded Space
City practice also opens the door for collaboration. In densely populated areas, therapists often work closely with local vets, hydrotherapists, behaviourists, and trainers. Holistic care becomes a team effort, especially when addressing complex cases such as post-surgical recovery, chronic pain, or anxiety-related musculoskeletal issues.
An osteopath may refer a reactive dog for behavioural therapy to reduce stress-related tension or consult with a vet on pain management options. The ability to build interdisciplinary partnerships enhances care and helps avoid siloed treatment plans.
Behavioural Therapies and Emotional Health
Urban life doesn’t just affect the physical body; it taxes the nervous system too. Many holistic practitioners, including osteopaths, incorporate trauma-informed approaches and work with the parasympathetic nervous system. Cranial techniques and gentle fascia work can help soothe overly aroused or anxious pets, supporting emotional regulation as much as physical release.
When combined with behaviour therapy, enrichment, and environmental changes, these hands-on techniques can have a profound impact on an animal’s quality of life.
Supporting the Urban Vet: Osteopathy as a Complementary Tool
Urban veterinarians are on the frontlines of animal care in often high-pressure, high-volume settings. With limited consultation time and increasingly complex client expectations, they face significant challenges: managing chronic pain cases, addressing behavioural issues linked to physical discomfort, and meeting the rising demand for holistic care options.
In these contexts, osteopathy can offer meaningful support. For vets, gaining training in animal osteopathy or working in tandem with a qualified osteopath opens up new treatment pathways, particularly for musculoskeletal complaints, compensatory gait patterns, and unresolved lameness cases where conventional diagnostics may show limited findings.
Collaborative work with osteopaths can also reduce the burden of long-term pharmaceutical management by supporting natural healing processes, improving mobility, and enhancing the animal’s comfort and function. This integrative model aligns well with modern veterinary medicine’s shift toward multimodal care and can improve both clinical outcomes and client satisfaction.
Moreover, offering or referring to osteopathic treatment can help urban clinics stand out in competitive markets, responding to a growing client base seeking evidence-informed complementary therapies. With appropriate training and clear referral frameworks, osteopathy becomes a valuable asset in the urban vet’s toolkit.
Looking Ahead: Education and Awareness
As urban pet ownership continues to rise, so too does awareness of proactive, preventative care. Increasingly, city owners are seeking out holistic and complementary therapies not only for recovery from injury but for ongoing wellness. There’s a growing recognition that bodywork isn’t indulgent; it’s essential.
For animal osteopaths and holistic therapists, urban practice offers a rich and rewarding opportunity to make a real difference. It requires creativity, empathy, and a deep understanding of the urban animal’s world. But in return, it brings the chance to help pets thrive, one borough, one body at a time.
References
- Taylor, M., & Mills, D. (2007). The effect of the kennel environment on canine welfare: A critical review of the literature. Animal Welfare, 16(4), 435–447.
- Brown, D. C., Boston, R. C., Coyne, J. C., & Farrar, J. T. (2008). A novel approach to the use of animals in studies of pain: Validation of the canine brief pain inventory in canine osteoarthritis. Pain Medicine, 9(4), 434–442.
- McGreevy, P. D., & Nicol, C. J. (1998). The importance of ethology in understanding the behaviour of the horse. Equine Veterinary Journal, 30(1), 15–19.
- Haussler, K. K., & Frisbie, D. D. (2009). The role of manual therapy in equine physical rehabilitation. Veterinary Clinics of North America: Equine Practice, 25(1), 109–122.
- Franklin, S. H., Naylor, R. J., Lane, J. G., & Starling, M. J. (2018). Canine behaviour problems: Discussions between veterinarians and dog owners during annual booster consultations. Journal of Small Animal Practice, 59(3), 161–167.
- Mills, D. S., & Hall, S. S. (2014). Animal-assisted interventions: Making better use of the human–animal bond. Veterinary Record, 174(11), 269–273.
- King, A. S., & Mansmann, R. A. (2003). Manual therapy and complementary techniques in veterinary medicine. In Veterinary Clinics of North America: Small Animal Practice, 33(6), 1329–1347.
Benefits of Osteopathy for the Care and Treatment of the Geriatric Equine
Click on the thumbnail below to read an exemplary thesis by LCAO International Diploma in Canine Osteopathy student, Sharon Ferrer, in which she examines the efficacy of regular osteopathic treatments on anxiety in dogs.
For more information on how you can become an Animal Osteopath, click here